Do you forget things the odd time? Can’t pull the right word from your memory bank? Walk into a room and forget what you were after? Well, it could be the very early stages of Alzheimer’s disease that you’re experiencing or just a busy day in a hectic life.
How do you know the difference? You don’t. At least not in the early stage, called preclinical Alzheimer’s disease. Unless there is a family history or some other reason, your family physician is unlikely to order the test that would scan your brain for amyloid beta which is a deposit of protein found in the brains of Alzheimer’s sufferers.
Not all people with some form of mild cognitive impairment have Alzheimer’s disease but the same tests that can diagnose preclinical Alzheimer’s disease can also rule it out.
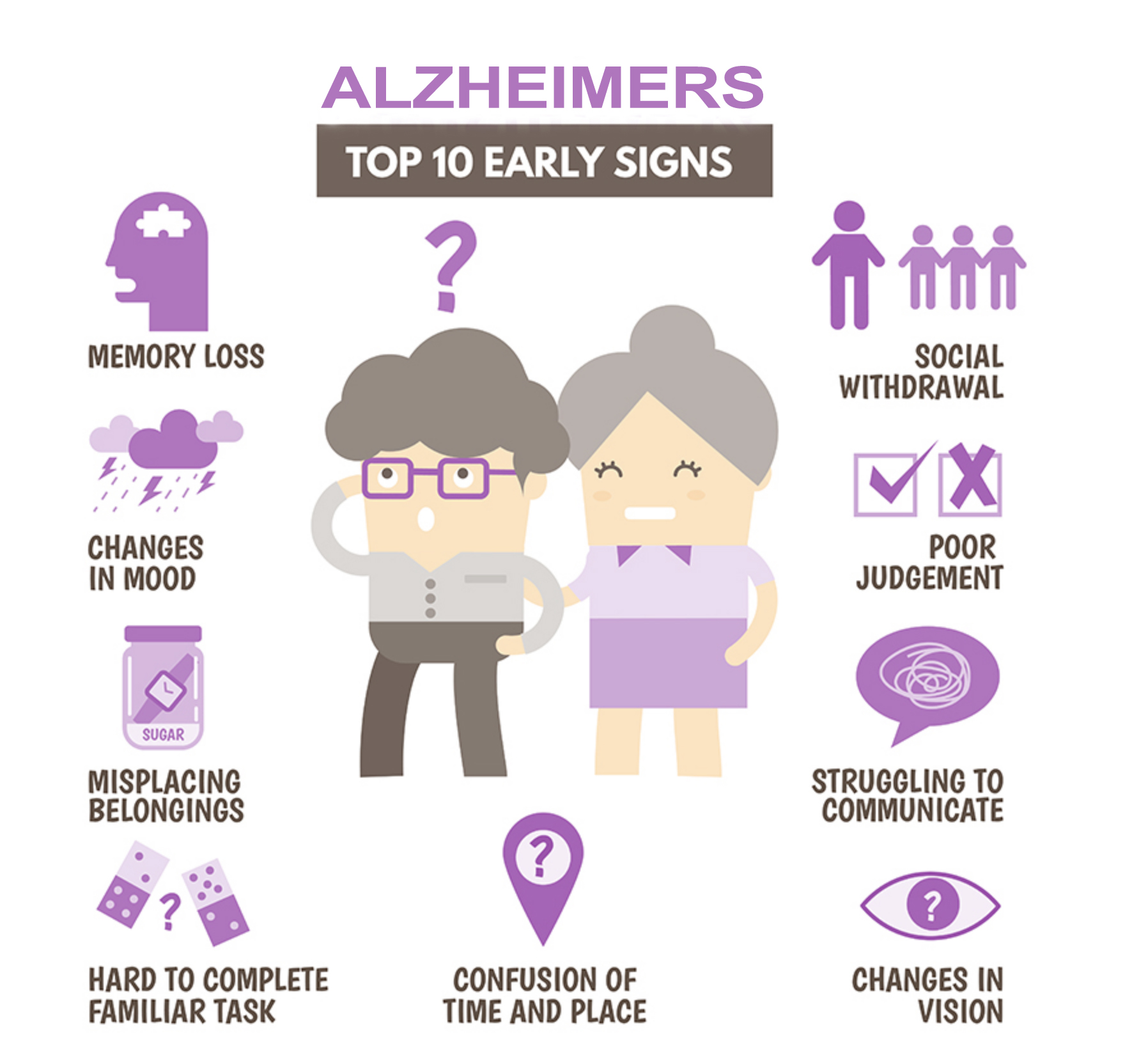
The stage of preclinical Alzheimer’s disease can continue for many years and, while some develop coping skills or attribute symptoms to a busy life, others will notice increasing difficulties with memory, attention span, communication, problem solving or mood swings.
Alzheimer’s disease is generally diagnosed in the mild dementia stage when tasks such as making decisions or planning a family event become challenging, when a person finds familiar surroundings unfamiliar at times or when changes in personality become more consistently noticeable. Once diagnosed, a variety of supports can be put in place to keep the individual safe and to help him or her navigate their world a bit better. At this point, Alzheimer’s sufferers are generally able to stay in their own homes. Technologies such as the GPS capabilities of smart phones combined with low tech interventions like labeling the contents of cupboards and drawers or alarm reminders can be effective to help reduce confusion and combat caregiver stress.
The moderate or middle stage of Alzheimer’s disease brings a greater decline in both functional and cognitive abilities. Some degree of assistance will be needed with daily living tasks such as showering, dressing and toileting. The repetition of stories and mistaking one person for another or forgetting who family members are altogether is common. The personality changes associated with Alzheimer’s disease become more pronounced in this stage. Agitation, suspiciousness and restlessness are common. As a person’s disease descends into this stage, it becomes increasingly challenging to manage them at home. Caregivers can begin to find their own health impacted, Alzheimer’s sufferers may put their own safety at risk unintentionally and home care workers or other caregiving relievers may be few and far between.
Late stage Alzheimer’s brings a further decline in cognitive and functional abilities. At this point complete assistance is generally required for everything from eating to dressing and toileting. The ability to process information or communicate is severely impacted as is the ability to walk without help or even hold up one’s head. For the family and close friends of an Alzheimer’s patient, this stage may feel like the person is lost to them but there is good evidence that there are at least moments when the person they knew shines through. Music programs have been able to encourage the singing of familiar old songs, therapy dogs have encouraged speech in patients who don’t talk any longer and a familiar smell may bring back memories.
Alzheimer’s disease is very complex but effects of the disease such as the inability to take in sufficient nutrients due to difficulty swallowing or the body’s inability to fight off infection leads to other life-threatening conditions. People don’t die of Alzheimer’s disease as such, rather they die of lung infections, multi-organ failure, strokes or heart attacks. The goal of treatment at this point centers around quality of life and comfort.
For more information about Alzheimer’s disease including what to expect, how to prepare and tips for caregivers follow this link to Alzheimer’s Society of Canada.
Do you know the stages of Alzheimer's disease? Share on X




Add Your Voice
0 Comments
Join the Discussion